Eliminating Diseases Vaccines & Human History


Eliminating Diseases Objectives
-
List examples of human-to-human, vector, and environmental infectious disease transmission.
-
Describe the pathogens, form of transmission, and symptoms associated with smallpox and polio.
-
Explain how vaccines work and why they are critical in controlling infectious diseases.

A key to addressing infectious diseases is to adequately understand transmission.
Many day-to-day activities, like washing hands and cooking food, are intended in part to reduce disease transmission.

Infectious disease transmission can be broken into three categories.

Human to Human

Vector

Environmental

There are numerous ways an infectious disease agent can be transmitted to a human. Some of these are more obvious, others have more obscure names. Iatrogenic transmission means through a medical procedure like using a needle or a blood product. Vertical transmission refers to a mother transmitting to a baby immediately before or after birth.
We often hear about food recalls due to pathogens like salmonella or E. coli. This poster provides a structure for thinking about food-borne pathogens.
SARS-CoV-2 Transmission
We have received many excellent questions about COVID-19 and the virus SARS-CoV-2. Several of these questions and answers are located throughout this module, matched with each topic.

Q. If I someone is unvaccinated or immunocompromised, do they need to wear a mask if 6 feet away from people?
A. Short answer is possibly. There are multiple factors at play here. First, research indicates that this virus spreads further than six feet away from its host. This is a small virus that can remain airborne for a period of time. Variables include location (indoors vs. outdoors), air currents, dispersal force (breathing, talking, sneezing), and the time spent within the range of an infected individual. Additional variables may be the type of mask, the fit of the mask, and mask handling. Also, research on use of masks indicates that masks are not 100% effective in stopping infection, some health care workers became infected wearing fitted quality masks. However masks do drop infection rate significantly. Also at play is the health of the individual in how significant an infection can become. This is a case where consulting a health care professional familiar with an individual’s medical situation can be advantageous.
Q. If the primary form of covid transmission is respiratory why did we wash everything?
A. This is a good question, and it has to do with the time it takes to learn about a new pathogen and concerns about reducing the percentage of risk in the mean time. Staying a distance away from other people reduces risk for transmission of many infectious diseases, wearing a mask reduces risk even more. Not touching the eyes, nose, or mouth, reduces risk. Washing hands after touching an object that may have a virus on it may have shaved off even more risk potential. Think of it as a game, and you want the risk of exposure to drop from 100% to as close to 0% as possible without a significant drop in quality of life. One behavior may not be adequate, the risk remains too high. Combining multiple behaviors drops the risk lower and lower. Practicing all of the risk-reducing behaviors all the time has you prepared for changing circumstances. Although research now supports that covid-19 is primarily spread through respiratory transmission, reduction of the spread of other pathogens like influenza and rhinoviruses reduces occurrence of other impactful diseases.

You are not just protecting yourself, you are protecting everyone you contact, including family and friends.
We are now well aware of the significance of having a vaccine that builds defenses against SAR-CoV-2. Smallpox, Polio, and AIDS serve as case studies for the benefits and issues associated with developing and distributing effective vaccines.
Smallpox (caused by Variola virus)
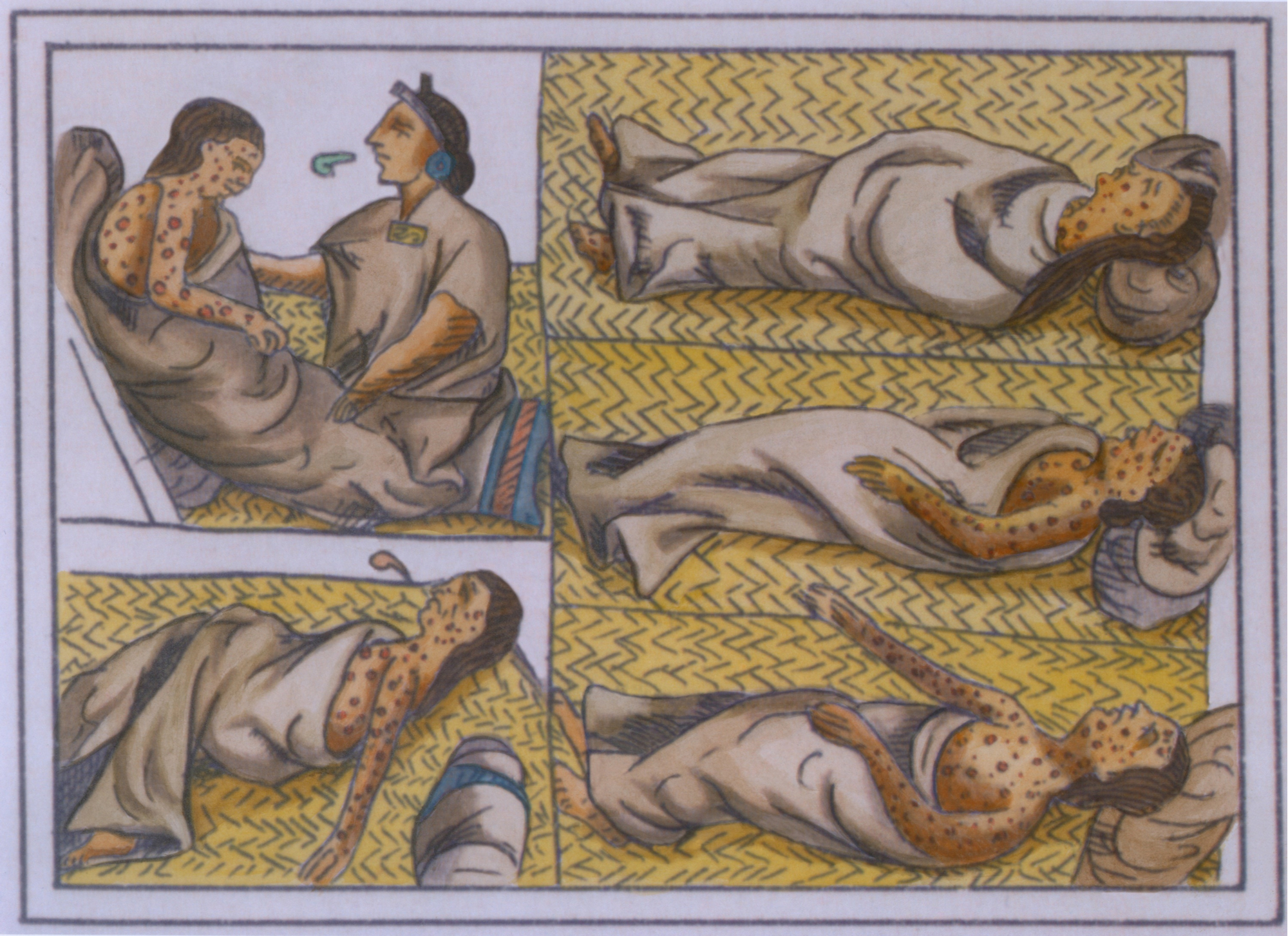
Smallpox terrorized people for thousands of years. It crept though populations, killing many, and leaving many others suddenly blind and scarred from head to toe. Smallpox may also have been the earliest example of a pathogen used as a form of biological weapon.
And now it is gone. This is one of the most amazing stories in human history.

Polio (caused by Poliovirus)

Polio, like Smallpox, is a disease that has impacted humans world-wide for thousands of years. However, even though we have an effective vaccine and have tried to eradicate polio since the 1980s, some cases still exist. This is a story of resources, medical infrastructures, and conflict.
This video provides a context for the battle against poliovirus.

In 2018, the number of “wild” polio cases (cases not related to symptoms after receiving the vaccine) dropped under 100 cases. However, the cases rose to over 200 in 2019. Conflict, resistance to vaccination programs, and limitations in medical infrastructure have hampered vaccine distribution.
We are waiting for 2022 data, COVID has complicated polio vaccination and overall disease reporting.
COVID-19 and Inequality

Q. Why are older people, and individuals with some pre-existing medical conditions, more likely to develop life-threatening cases of COVID?
A. Excellent question, and one still under research. There are most likely numerous reasons for discrepancy related to age and health, including less immune response or delayed and inappropriate immune response. Men also appear to have a higher mortality rate than women which is not yet understood. One area under research is the process of a “cytokine storm,” a release of the chemicals from wounded cells that trigger an inflammation response. Too much inflammation can lead to too much blood leaking from vessels, organ failure, and shock. Since the virus can impact multiple organ systems, individuals with pre-existing health conditions like cardiovascular diseases and diabetes can develop worsening symptoms rapidly.
The Need for Vaccines
In controlling infectious diseases, an effective vaccine is the “gold standard” for reducing significant infections.

An important aspect of vaccination that is often overlooked is that this is not necessarily a process for a particular individual; this is for society. Some people can not be immunized because they are too young, too ill, or have a compromised immune system. If everyone else is vaccinated, this provides “herd immunity” that protects the most vulnerable people from being exposed to the pathogen.

There can be significant challenges in developing and distributing effective vaccines. An effective vaccine has few side effects, causes the body to produce sufficient and lasting memory cells, and is cost effective.
In the case of COVID-19, the aim was rapid vaccine development to reduce hospitalization and death, with minimal vaccine side effects. The hope was to vaccinate everyone possible to create rapid herd immunity. However, lower vaccination rates, viral mutations, and not developing lasting memory cells means vaccine boosters will be needed for the foreseeable future.
One of the most researched vaccines is against strains of influenza. The flu virus mutates at a rapid rate and has the potential to cause pandemics as occurred in 1918 with the “Spanish flu” that killed tens of millions of people in a year’s time.

This video provides information about influenza infections. If you have had the flu, you are probably well aware that symptoms can be severe.
Altered viral antigens can result in memory cells no longer recognizing the pathogen when it enters the body.
Covid Vaccine

Q. What questions remain about the new covid-19 vaccines?
A. The vaccines against covid-19 have been shown to reduce the risk for severe illness and death from SARS-CoV-2. Questions remain about how frequently boosters will be needed, and whether they will be effective against emerging viral variants. It takes time to study vaccine efficacy. A vaccine was not developed for SARS-CoV-1 since a combination of luck and strict quarantining stopped the spread. As a result, we do not know how vaccines against SARS will function over extended periods of time.
If you would like to learn more about the original SARs outbreak, there are archived CDC web pages available.
Q. Will quarantining be over for good, now that we have a vaccine and boosters?
A. Herd immunity is the idea that enough people are not carrying an active pathogen so those who are not vaccinated like immunocompromised or the very young are not exposed to the pathogen. The goal is to reach a significant number of people, 85 to 90% who have memory cells either from being directly infected, or in a less risky manner, from a vaccine. They are less likely to carry enough viral load to infect other people. An effective vaccine would have to be administered widely to people who have not been exposed to the virus, and that is taking time. Repeated infections, even in the vaccinated is indicating short “memory” of the virus. Even if a vaccinated person does not get severely ill, they could pass the virus to someone who is unvaccinated and at risk for severe illness. Additionally new variants may lead to future quarantines.

The next section provides a closer look at infectious diseases that have remained persistent threats to our species.

Check your knowledge. Can you:
-
list examples of human-to-human, vector, and environmental infectious disease transmission?
-
describe the pathogens, form of transmission, and symptoms associated with smallpox and polio?
-
explain how vaccines work and why they are critical in controlling infectious diseases?